
-
Enquiry | Appointment
022-66776677 | +91-8779678354 -
Surgery | Bookings
+91-7208286076 | 022-66776677 -
Email
contact@envisioneyehospital.in
Retinal Diseases-Overview
Retinal diseases vary widely, but most of them cause visual symptoms. Retinal diseases can affect any part of your retina, a thin layer of tissue on the inside back wall of your eye.
The retina contains millions of light-sensitive cells (rods and cones) and other nerve cells that receive and organize visual information. Your retina sends this information to your brain through your optic nerve, enabling you to see.
Treatment is available for some retinal diseases. Depending on your condition, treatment goals may be to stop or slow the disease and preserve, improve or restore your vision. Untreated, some retinal diseases can cause severe vision loss or blindness.
Types
Common retinal diseases and conditions include:
- Retinal tear A retinal tear occurs when the clear, gel-like substance in the center of your eye (vitreous) shrinks and tugs on the thin layer of tissue lining the back of your eye (retina) with enough traction to cause a break in the tissue. It's often accompanied by the sudden onset of symptoms such as floaters and flashing lights.
- Retinal detachment A retinal detachment is defined by the presence of fluid under the retina. This usually occurs when fluid passes through a retinal tear, causing the retina to lift away from the underlying tissue layers.
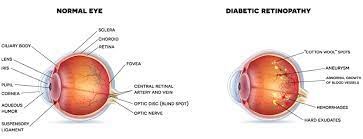
- Diabetic retinopath If you have diabetes, the tiny blood vessels (capillaries) in the back of your eye can deteriorate and leak fluid into and under the retina. This causes the retina to swell, which may blur or distort your vision. Or you may develop new, abnormal capillaries that break and bleed. This also worsens your vision.
- Epiretinal membrany. Epiretinal membrane is a delicate tissue-like scar or membrane that looks like crinkled cellophane lying on top of the retina. This membrane pulls up on the retina, which distorts your vision. Objects may appear blurred or crooked.
- Macular holep A macular hole is a small defect in the center of the retina at the back of your eye (macula). The hole may develop from abnormal traction between the retina and the vitreous, or it may follow an injury to the eye.
- Macular degeneration In macular degeneration, the center of your retina begins to deteriorate. This causes symptoms such as blurred central vision or a blind spot in the center of the visual field. There are two types — wet macular degeneration and dry macular degeneration. Many people will first have the dry form, which can progress to the wet form in one or both eyes.
- Retinitis pigmentosa Retinitis pigmentosa is an inherited degenerative disease. It slowly affects the retina and causes loss of night and side vision.
Signs and Symptoms
- Seeing floating specks or cobwebs
- Blurred or distorted (straight lines look wavy) vision
- Defects in the side vision
- Lost vision
You may need to try looking with each eye alone to notice these.
Risk Factors
- Aging
- Smoking
- Being obese
- Having diabetes or other diseases
- Eye trauma
- A family history of retinal diseases
Diagnosis
To make a diagnosis, we conduct a thorough eye exam and looks for abnormalities anywhere in the eye. The following tests may be done to determine the location and extent of the disease:
- Amsler grid test Amsler grid is used to test the clarity of your central vision. We will ask you if the lines of the grid seem faded, broken or distorted and will note where the distortion occurs on the grid to better understand the extent of retinal damage. If you have macular degeneration, doctor might also ask you to use this test to self-monitor your condition at home.
- Optical coherence tomography (OCT) This test is an excellent technique for capturing precise images of the retina to diagnose epiretinal membranes, macular holes and macular swelling (edema), to monitor the extent of age-related wet macular degeneration, and to monitor responses to treatment.
- Fundus autofluorescence (FAF) FAF may be used to determine the advancement of retinal diseases, including macular degeneration. FAF highlights a retinal pigment (lipofuscin) that increases with retinal damage or dysfunction.
- Fluorescein angiography This test uses a dye that causes blood vessels in the retina to stand out under a special light. This helps to exactly identify closed blood vessels, leaking blood vessels, new abnormal blood vessels and subtle changes in the back of the eye.
- Indocyanine green angiography This test uses a dye that lights up when exposed to infrared light. The resulting images show retinal blood vessels and the deeper, harder-to-see blood vessels behind the retina in a tissue called the choroid.
- Ultrasound This test uses high-frequency sound waves (ultrasonography) to help view the retina and other structures in the eye. It can also identify certain tissue characteristics that can help in the diagnosis and treatment of eye tumours.
- CT and MRI In rare instances these imaging methods can be used to help evaluate eye injuries or tumours.
Treatment
The main goals of treatment are to stop or slow disease progression and preserve, improve or restore your vision. In many cases, damage that has already occurred can't be reversed, making early detection important. Doctor work with you to determine the best treatment.
- Using a laser. Laser surgery can repair a retinal tear or hole. We use a laser to heat small pinpoints on the retina. This creates scarring that usually binds (welds) the retina to the underlying tissue. Immediate laser treatment of a new retinal tear can decrease the chance of it causing a retinal detachment.
- Shrinking abnormal blood vessels. use a technique called scatter laser photocoagulation to shrink abnormal new blood vessels that are bleeding or threatening to bleed into the eye. This treatment may help people with diabetic retinopathy. Extensive use of this treatment may cause the loss of some side (peripheral) or night vision.
- Freezing. In this process, called cryopexy, we apply a freezing probe to the external wall of the eye to treat a retinal tear. Intense cold reaches the inside of the eye and freezes the retina. The treated area will later scar and secure the retina to the eye wall.
- Injecting air or gas into your eye. This technique, called pneumatic retinopexy, is used to help repair certain types of retinal detachment. It can be used in combination with cryopexy or laser photocoagulation.
- Indenting the surface of your eye. This surgery, called scleral buckling, is used to repair a retinal detachment. We sew a small piece of silicone material to the outside eye surface (sclera). This indents the sclera and relieves some of the force caused by the vitreous tugging on the retina and reattaches the retina. This technique may be used with other treatments.
- Evacuating and replacing the fluid in the eye. In this procedure, called vitrectomy, surgeon removes the gel-like fluid that fills the inside of your eye (vitreous), then injects air, gas or liquid into the space. Vitrectomy may be used if bleeding or inflammation clouds the vitreous and obstructs the surgeon's view of the retina. This technique may be part of the treatment for people with a retinal tear, diabetic retinopathy, a macular hole, epiretinal membrane, an infection, eye trauma or a retinal detachment.
- Injecting medicine into the eye. Doctor may suggest injecting medication into the vitreous in the eye. This technique may be effective in treating people with wet macular degeneration, diabetic retinopathy or broken blood vessels within the eye.
- Implanting a retinal prosthesisPeople who have severe vision loss or blindness owing to certain inherited retinal disease may need surgery. A tiny electrode chip is implanted in the retina that receives input from a video camera on a pair of eyeglasses. The electrode picks up and relays visual information that the damaged retina can no longer process.
Why you can choose Retinal Treatment with us?
Our centre is well equipped with modern technology to diagnose and treat a multitude of vitreo retinal conditions. Treatment includes both medical and surgical interventions.
State-of-the-art equipment for investigation and diagnosis of various Vitreo retinal diseases include:
- Fundus Fluorescein Angiography (FFA) and Indocyanine Green Angiography (ICGA)
- Optical Coherence Tomography (OCT)
- Ultrasonography
- Ultrasound Bio Microscopy (UBM)
- Electroretinogram (ERG)including Multifocal (mfERG), Visual Evoked Potential (VEP), Electro Oculo Graphy (EOG)
Medical and Surgical management for various retinal conditions like
- Diabetic Retinopathy,
- retinal vein occlusion (CRVO & BRVO),
- Arterial occlusion (CRAO),
- Central serous retinopathy (CSR),
- Age-related Macular Degeneration (AMD) etc.,
The centre is equipped with retinal lasers (Green laser – Double frequency YAG) with slit-lamp and indirect ophthalmoscopy delivery for treatment of these retinal conditions.
In addition, various intravitreal injections of Anti-VEGF drugs and steroids are used to treat macular edema as well as choroidal neovascular membranes (CNVM). Specialised lasers like trans pupillary thermotherapy (TTT) and photodynamic therapy (PDT) are also available.
The electrodiagnosis with genetic analysis support for retinal degenerations, along with guidance and referral for rehabilitation centres.
We are also involved in screening for Retinopathy of Prematurity (ROP) at base clinics as well as NICUs in other hospitals. Various paediatric retinal conditions like FEVR, PFV, tumours etc are also treated regularly.
We have operating theatres equipped with state-of-the-art vitrectomy machines, lasers and microscopes with posterior visualisation systems. Complex vitreo-retinal surgeries for repair of retinal detachment, diabetic tractional detachment, vitreous haemorrhage, macular holes and epiretinal membranes are routinely performed. Surgeries to manage intra-ocular foreign bodies and treatment of endophthalmitis are also routinely done.
